In a groundbreaking development that could redefine aging research, scientists are exploring the potential of CAR-T cell therapy to target and eliminate senescent cells—the so-called "zombie cells" that accumulate with age and contribute to tissue dysfunction. This innovative approach, dubbed "immune surveillance of aging," leverages the body’s own immune system to combat the ravages of time, offering a tantalizing glimpse into a future where age-related decline could be slowed or even reversed.
The Rise of Zombie Cells and the Aging Process
Senescent cells are cells that have entered a state of permanent growth arrest, refusing to die but no longer contributing to tissue function. Over time, these cells accumulate in organs throughout the body, secreting inflammatory molecules that disrupt neighboring healthy cells and fuel chronic low-grade inflammation—a hallmark of aging. While the immune system naturally clears some of these cells, its efficiency declines with age, allowing senescent cells to build up and accelerate tissue deterioration. This phenomenon has been linked to a range of age-related diseases, from osteoarthritis and atherosclerosis to neurodegenerative disorders.
CAR-T Cells: A Precision Strike Against Senescence
Chimeric antigen receptor (CAR) T-cell therapy, originally developed to treat cancers, is now being repurposed to tackle senescence. The therapy involves extracting a patient’s T cells, engineering them to express receptors that recognize specific markers on target cells, and then reinfusing them into the body. In cancer treatment, these receptors are designed to lock onto tumor antigens. For aging, researchers are identifying unique surface proteins expressed by senescent cells, enabling CAR-T cells to hunt them down with precision. Early studies in mice have shown remarkable results, with treated animals exhibiting improved organ function and extended healthspan.
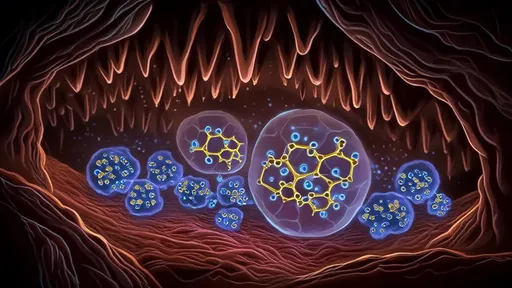
Overcoming the Challenges of Immune Evasion
One of the major hurdles in targeting senescent cells is their ability to evade the immune system. Unlike cancer cells, which often overexpress recognizable antigens, senescent cells are more heterogeneous and can cloak themselves from immune detection. To address this, scientists are developing multi-targeted CAR-T therapies that recognize several senescence-associated markers simultaneously. Another strategy involves combining CAR-T cells with senolytic drugs—compounds that weaken senescent cells, making them more vulnerable to immune attack. These synergistic approaches could enhance the efficacy of the treatment and reduce the likelihood of resistance.
Safety Concerns and the Risk of Off-Target Effects
While the potential of CAR-T therapy for aging is immense, safety remains a critical consideration. Senescent cells share some markers with healthy cells, raising concerns about off-target effects where engineered T cells might attack normal tissues. Researchers are employing advanced screening techniques to identify truly senescence-specific antigens and fine-tuning CAR-T designs to minimize collateral damage. Additionally, controlled dosing and "suicide switches"—genetic mechanisms to deactivate CAR-T cells if necessary—are being explored to ensure the therapy can be halted if adverse effects arise.
The Ethical and Economic Implications
Beyond the science, the advent of senescence-targeting CAR-T therapy raises broader questions. Who will have access to these potentially life-extending treatments, and at what cost? Current CAR-T therapies for cancer are prohibitively expensive, often exceeding hundreds of thousands of dollars per treatment. Scaling the technology for age-related applications will require significant cost reductions and equitable distribution models. Ethically, the prospect of significantly extending human healthspan challenges societal norms around aging, retirement, and resource allocation, necessitating proactive dialogue among scientists, policymakers, and the public.
A Glimpse Into the Future
If successful, CAR-T cell therapy for senescence could revolutionize how we approach aging, transforming it from an inevitable decline into a modifiable condition. Beyond treating age-related diseases, the technology might one day be used preventatively, administered periodically to clear senescent cells before they cause significant damage. While much work remains to translate these findings from mice to humans, the convergence of immunology and geroscience has never been more promising. For now, the idea of reprogramming our immune systems to sweep away the detritus of aging remains a bold and inspiring vision—one that inches closer to reality with each passing discovery.
By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025
By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025

By /Jul 29, 2025